Insulin and glucagon are the two key hormones involved in regulating your blood sugar levels. Most people rarely give them a second thought, but if you have diabetes or pre-diabetes, you know the significant influence these hormones can have on your health.
When blood sugar is not properly regulated, it can lead to various health complications – some of which can be life-threatening if unaddressed.
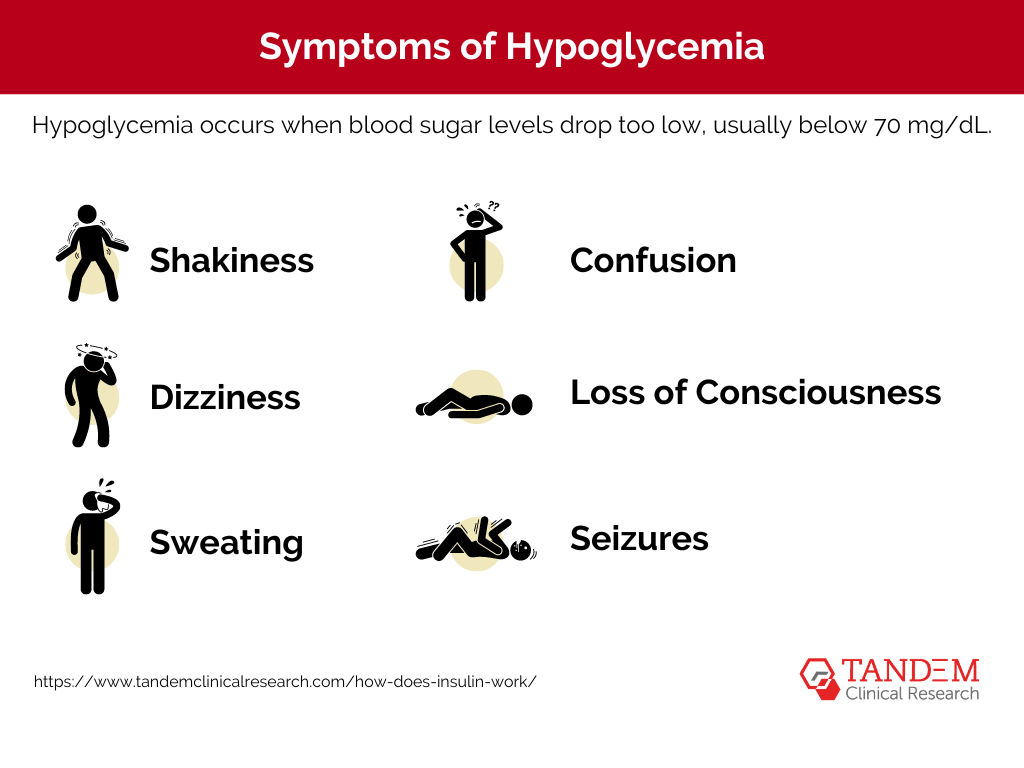
If blood sugar levels are consistently too high, a condition known as hyperglycemia occurs, a hallmark of diabetes mellitus. Conversely, if blood sugar levels drop too low, a condition called hypoglycemia occurs, causing shakiness, dizziness, confusion, and many other symptoms.
How exactly do insulin and glucagon play a role in all this? Let’s talk about it.
In this blog post, we’re diving into the endocrine system and its role in regulating blood sugar, both in people with diabetes and the rest of the population.
How Does Insulin Work?
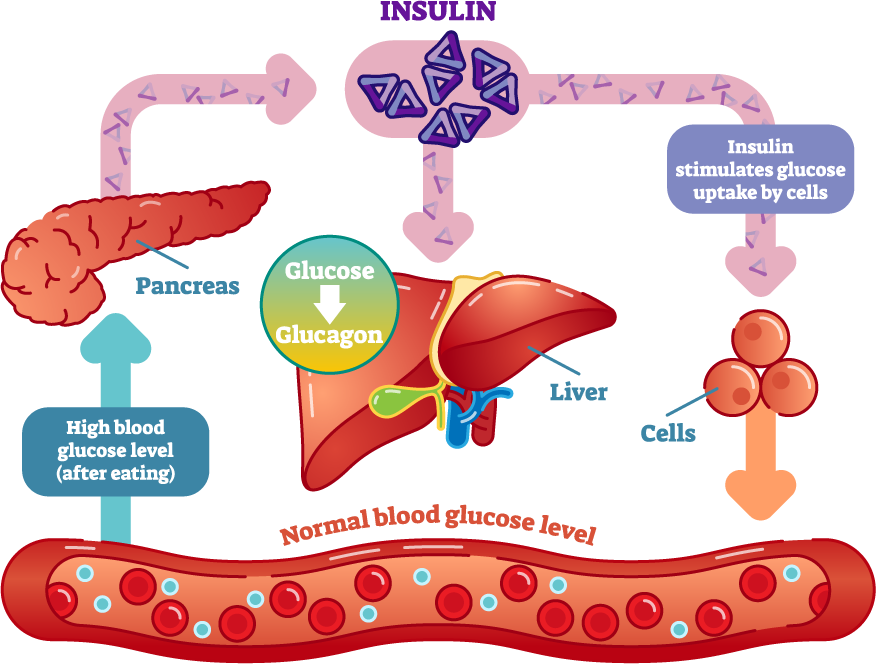
Insulin plays a pivotal role in regulating glucose metabolism in the body.
Its primary function is to facilitate the uptake of glucose from the bloodstream into cells, where it can be used for energy or stored for later use. It achieves this by binding to insulin receptors on the surface of target cells, particularly muscle, fat, and liver cells.
Once insulin binds to its receptor, it triggers a series of intracellular signaling pathways that ultimately lead to the translocation of glucose transporter proteins to the cell membrane. These transporter proteins act as channels through which glucose can enter the cell.
Insulin also plays a crucial role in suppressing glucose production by the liver and promoting the storage of excess glucose as glycogen. Additionally, it stimulates the conversion of glucose into fatty acids for storage in adipose tissue.
Several factors that can influence the function of insulin in your body. One of the most common is your blood glucose levels.
Insulin secretion is tightly regulated in response to changes in blood glucose levels. When blood glucose levels rise, the pancreas releases insulin to facilitate glucose uptake by cells.
On the other hand, when blood glucose levels drop, insulin secretion decreases, allowing the liver to release glucose into the bloodstream.
What Does Glucagon Do?
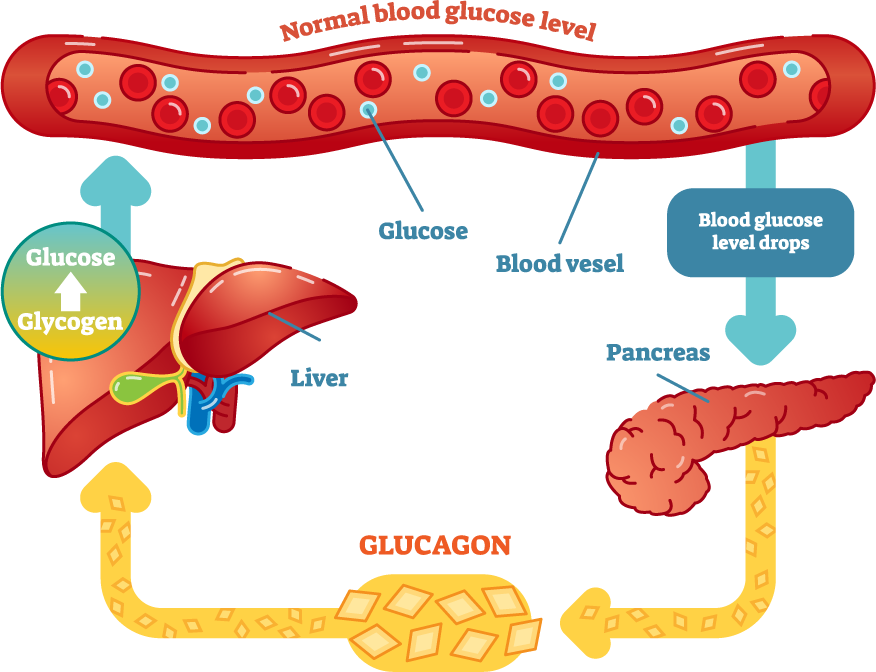
Glucagon is a hormone produced by the alpha cells of the pancreas, and it serves as a crucial counterpart to insulin in regulating glucose homeostasis, which is the process of maintaining a stable level of blood sugar.
While insulin works to lower blood sugar levels by promoting glucose uptake into cells, glucagon works to increase blood sugar levels when they fall too low. It stimulates the breakdown of glycogen into glucose, a process called glycogenolysis.
Glycogen is a storage form of glucose, and when blood sugar levels drop, glucagon signals the liver to release glucose from glycogen stores into the bloodstream. This helps to raise blood sugar levels and provide a steady supply of glucose to cells, particularly the brain and nervous system, which rely heavily on glucose for energy.
Glucagon also stimulates gluconeogenesis, the production of glucose from non-carbohydrate sources such as amino acids and glycerol. This further helps replenish blood glucose levels during times of fasting or prolonged exercise.
The secretion and function of glucagon are influenced by several factors, including your insulin levels. As we explained, insulin lowers blood sugar levels while glucagon raises them.
Therefore, insulin inhibits the secretion of glucagon, and glucagon inhibits the secretion of insulin, creating a delicate balance between the two hormones – but let’s explore this relationship even more.
How Insulin and Glucagon Interact
The bottom line is that insulin and glucagon work together in a tightly regulated system to maintain blood sugar levels within a narrow range, ensuring that cells receive a steady supply of energy.
The actions of these two hormones are particularly critical during transitions between the fed state (postprandial) and the fasting state.
In the fed state, after a meal, blood glucose levels rise as a result of the digestion and absorption of carbohydrates. In response to the increase in blood glucose levels, the pancreas releases insulin.
Insulin promotes the uptake of glucose into cells, but it also inhibits the release of glucose from the liver and promotes the synthesis of fatty acids and protein, contributing to energy storage and tissue growth.
Conversely, in the fasting state, such as between meals or during prolonged periods of fasting, blood glucose levels begin to decline. In response to falling blood glucose levels, the pancreas reduces the secretion of insulin and increases the secretion of glucagon.
In summary, insulin and glucagon play complementary roles in regulating blood sugar levels in the body. Together, these hormones help to maintain blood sugar levels within a physiological range, ensuring that cells have a constant supply of energy to support metabolic processes and physiological functions.
The Implications of Insulin and Glucagon Dysregulation
Research indicates that dysregulation of insulin and glucagon can have significant implications for health, leading to conditions such as hyperglycemia and hypoglycemia, which are commonly associated with diabetes mellitus.
Diabetes (Type 1 & 2)
Hyperglycemia is characterized by elevated blood sugar levels, often resulting from insufficient insulin production or impaired insulin function. Generally, people experiencing chronically high blood sugar are also diagnosed with either type 1 or type 2 diabetes, depending on their circumstances.
In type 1 diabetes, which affects at least 5% of the U.S. population, the immune system attacks and destroys the insulin-producing beta cells in the pancreas. This leads to an absolute deficiency of insulin.
Without adequate insulin, glucose cannot enter cells, causing blood sugar levels to rise. Chronic hyperglycemia in type 1 diabetes can lead to complications such as cardiovascular disease, kidney damage, nerve damage, and vision problems if left untreated.
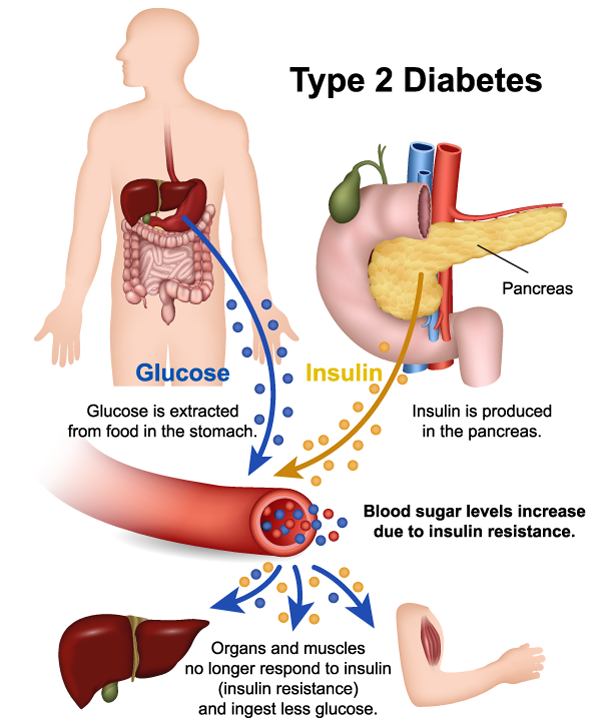
Present in roughly 38 million Americans – according to the Centers for Disease Control and Prevention – type 2 diabetes is characterized by insulin resistance, where cells become less responsive to insulin’s effects, and impaired insulin secretion by pancreatic beta cells. This results in elevated blood sugar levels due to reduced glucose uptake by cells and increased glucose production by the liver.
Type 2 diabetes is often associated with lifestyle factors such as obesity, physical inactivity, and poor diet. Unfortunately, once diagnosed, there is no cure for type 2 diabetes, but it can be managed through a range of treatment options.
If left untreated, type 2 diabetes can lead to similar complications as type 1 diabetes.
Low Blood Sugar
Hypoglycemia occurs when blood sugar levels drop too low, usually below 70 mg/dL. It can result from excessive insulin or other glucose-lowering medications, delayed or missed meals, excessive physical activity, or alcohol consumption.
This condition is especially common in people with diabetes. One study found that four in five people with type 1 diabetes and almost half of people with Type 2 diabetes who take insulin have experienced low blood sugar at least once in four weeks.
Symptoms of hypoglycemia include:
- Shakiness
- Dizziness
- Sweating
- Confusion
- Loss of consciousness
- Seizures
Prompt treatment of hypoglycemia involves consuming fast-acting carbohydrates, such as glucose tablets or fruit juice, to raise blood sugar levels quickly. In cases of severe hypoglycemia, glucagon injections may be necessary to raise blood sugar levels.
Overall, dysregulation of insulin and glucagon can lead to serious health consequences, highlighting the importance of maintaining balanced blood sugar levels, as well as properly managing both diabetes and hypoglycemia.
Help Researchers Study Insulin & Glucagon Interactions
Clinical trials play a vital role in advancing our understanding of how insulin works and in developing new treatments for blood sugar problems, including diabetes.
These studies are designed to investigate the safety and efficacy of potential therapies, as well as to explore the interactions between insulin and other hormones like glucagon.
Diabetes research studies often focus on various aspects of insulin function, including its role in glucose metabolism, its impact on blood sugar regulation, and its interactions with other hormones, such as glucagon.
In many cases, this involves testing new insulin formulations, delivery methods, or combination therapies aimed at improving blood sugar control and reducing the risk of complications associated with diabetes.
By participating in safe, professionally monitored clinical trials, patients with diabetes can contribute to the development of innovative treatments that may improve their own health outcomes and benefit future generations.
Get Matched With Tandem Clinical Research Today
We know a great deal about the relationship between insulin and glucagon, yet medical research continues to teach us more about how these key players interact and impact conditions like diabetes.
The more we can learn about the interplay between insulin and glucagon, the more efficiently we can treat the symptoms of type 1 and 2 diabetes, as well as hypoglycemia.
If you’re interested in contributing to diabetes clinical research, learn if you qualify for a study near you. Tandem Clinical Research will help you assess your options and enroll in the right trial.