
According to the Centers for Disease Control, around 3.1 million adults (1.3%) have inflammatory bowel disease in the United States. Despite the fact that it affects so many Americans, there’s still confusion around two different types of IBD—Ulcerative Colitis and Crohn’s disease. Although these diseases share similarities, they are not the same.
Sometimes it can be hard to tell Crohn’s and Ulcerative Colitis disease apart at first glance. However, there are notable contrasts in symptoms and treatments between the two diseases. They also affect different areas and depths of the digestive tract, leading to unique complications.
If you have IBD, understanding the differences between Ulcerative Colitis vs. Crohn’s is important. This blog post will dive deeper into their five key differences and explore treatment options.
Where Is the Inflammation Located?
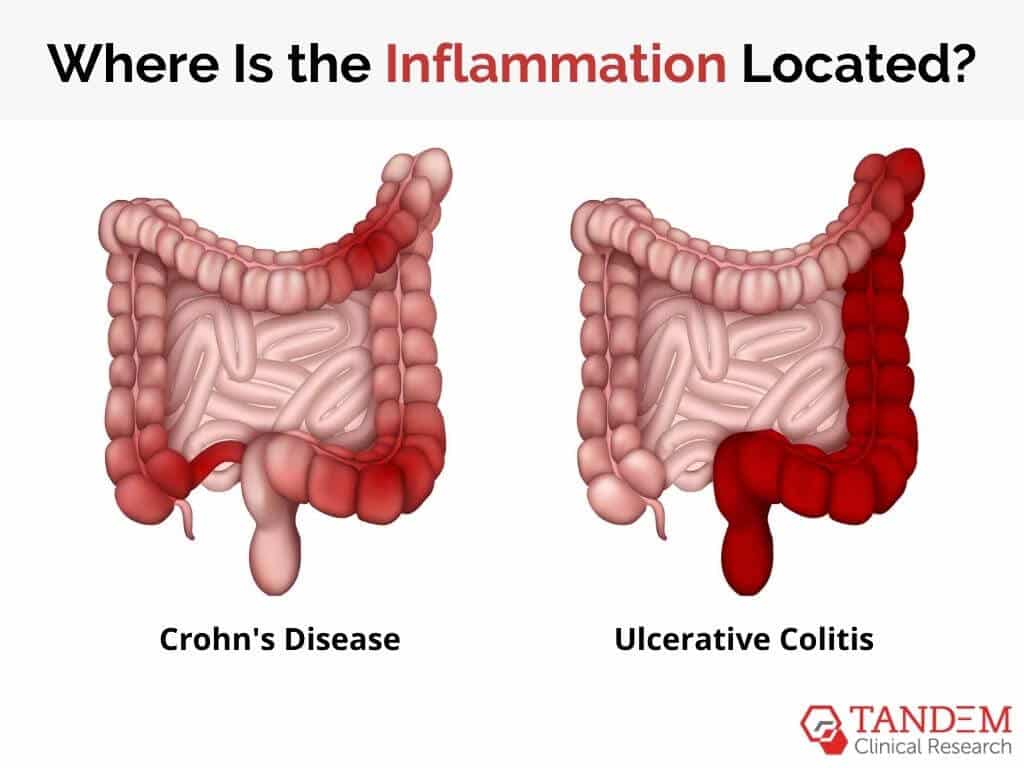
In both Crohn’s and ulcerative colitis, the inflammation affects the gastrointestinal tract. However, a key difference between these diseases is the precise location of the inflammation.
Crohn’s disease can occur anywhere along the gastrointestinal tract, which goes from the mouth to the anus. “Skip lesions” are common, where areas of disease are dispersed throughout the healthy tissue of the GI tract. In most cases, Crohn’s affects the portion of the small intestine that meets the large intestine.
On the other hand, ulcerative colitis specifically affects the colon and rectum. Depending on where the inflammation is located, there are different subsets of UC, like ulcerative proctitis or pancolitis.
The patient’s symptoms are the first indication of an inflammatory bowel disease. If a doctor suspects IBD, they first use blood tests to rule out other diseases, identify nutrient absorption issues, and signify inflammation. Stool samples can also indicate if high levels of inflammation are present.
For a proper IBD diagnosis, doctors primarily use imaging techniques like MRI, CT scans, colonoscopies, and capsule endoscopies. The pattern of disease (location and depth of inflammation) can often help differentiate between these two conditions.
Affected Layers of the Gastrointestinal Tract
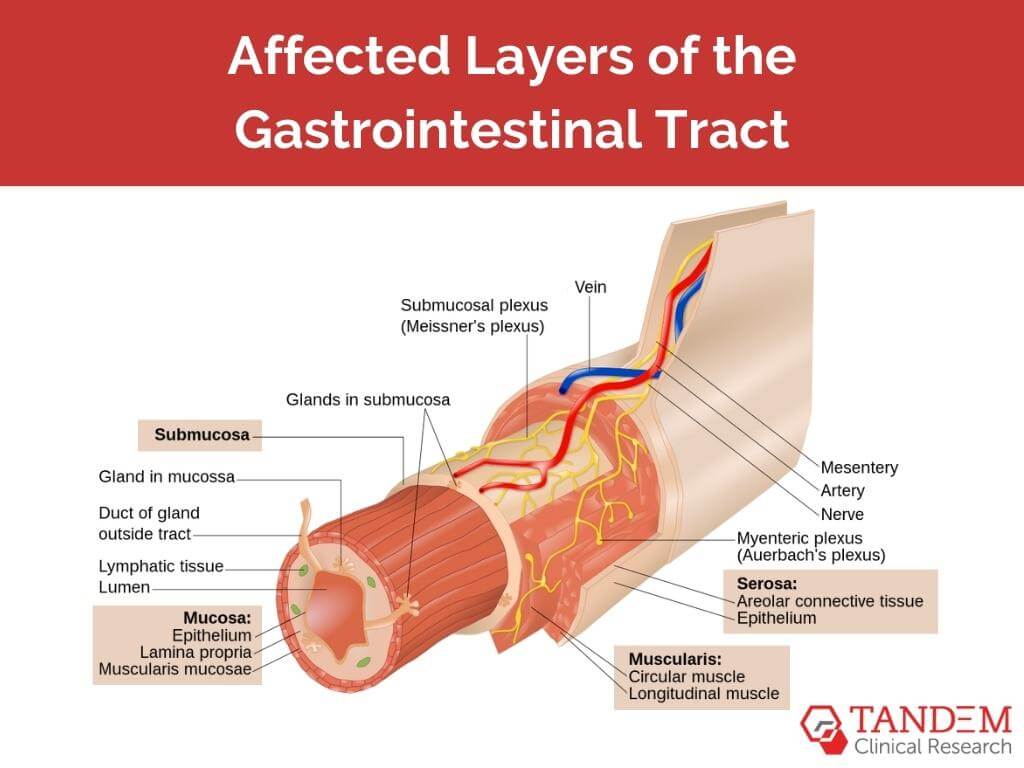
The gastrointestinal tract wall consists of four layers:
- the innermost mucosa,
- the submucosa
- the muscularis propria
- the outermost serosa
Crohn’s involves inflammation that extends through the entire thickness of the intestinal wall—from the innermost mucosa to the outermost serosa. This deep inflammation causes a range of complications. Fistulas, or abnormal connections between the intestine and organs, may form. They oftentimes result in swollen and painful infections called abscesses.
Additionally, inflammation and scar tissue can cause the intestines to swell and lead to blockages called strictures, which are relatively common for those diagnosed with Crohn’s disease. A 2010 study determined that 18.6% of patients with Crohn’s experienced stricturing complications 90 days after their diagnosis. Another 50% had complications after 20 years.
In contrast, ulcerative colitis primarily affects the innermost lining of the colon and rectum, called the mucosa. Chronic inflammation can cause ulcers that bleed–and rectal bleeding is very common for ulcerative colitis patients. They may also experience a toxic megacolon, which is a rare but dangerous complication.
Symptom Patterns
Although the two conditions do present with similar symptoms (abdominal pain, diarrhea, weight loss, and fatigue), there are patterns that separate Ulcerative Colitis vs Crohn’s disease.
For the most part, the symptoms of ulcerative colitis build over time. It usually begins to present itself with painful diarrhea that contains blood or pus. Since the disease mainly affects the rectum and colon, patients often experience rectal pain and bleeding. It’s also marked by the inability to defecate, despite having a strong urge to do so.
Like ulcerative colitis, Crohn’s disease symptoms often develop gradually. Some of the notable symptoms of Crohn’s include mouth sores, blood in stool, or painful leaking near the anus because of fistulas. Symptoms can also present in other areas, like the eyes, skin, and joints.
The symptoms specific to each disease also assist in diagnosis. For instance, the presence of a fistula, more common in Crohn’s, or the existence of persistent and bloody stool, more associated with ulcerative colitis, can suggest one diagnosis over the other.
Potential Complications

Both inflammatory bowel diseases share potential complications like malnutrition due to poor nutrient absorption or increased risk of colorectal cancer. However, certain complications of Ulcerative Colitis vs Crohn’s separate the two diseases.
Complications from Crohn’s include fistulas and abscesses resulting from its deep, transmural inflammation. The most common complications are strictures or intestinal obstructions caused by inflammation and scarring. Strictures lead to painful blockages in the GI tract. Severe strictures require surgery. If caught early, they can be fixed with medication.
Ulcerative colitis can lead to severe bleeding or a perforated colon. Severe bleeding is fairly common and can lead to anemia, requiring treatment. Perforation is less common but could require emergency care.
A toxic megacolon is a potentially deadly complication for ulcerative colitis patients. When a build-up of gas, swelling, and inflammation spreads throughout the colon, it can cause it to extend. If left untreated, the colon could rupture and result in death. Although rare, this is a dangerous condition that requires the immediate use of antibiotics, fluids, or tube feeding.
Treatment Options
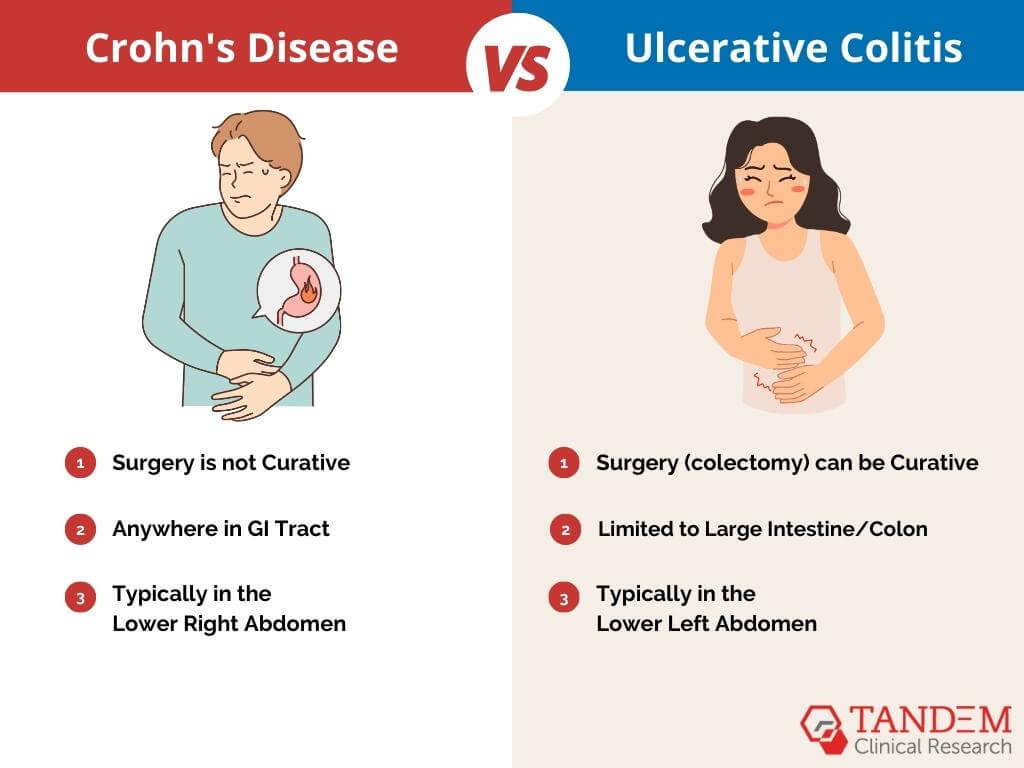
The treatments for Ulcerative Colitis and Crohn’s disease can overlap and vary.
Both kinds of IBD can be treated with medications to reduce inflammation and control symptoms. These include aminosalicylates, corticosteroids, and immunosuppressants. Biological therapies, like anti-TNF agents, may also be used but vary based on disease severity and patient response.
Treatment strategies diverge when considering surgery. Surgery (colectomy) can be curative in ulcerative colitis, as the disease is limited to the colon and rectum. This option is typically considered for patients with severe diseases unresponsive to medication or to prevent or address complications like cancer or toxic megacolon.
In Crohn’s, surgery is not curative, as the disease can occur anywhere in the GI tract and often recurs post-operation. Surgery, like bowel resection or strictureplasty, is mainly used to address complications like strictures, fistulas, or abscesses when they are unresponsive to medical management.
Thus, while medication is the mainstay of treatment for both, surgery plays a more definitive role in ulcerative colitis but is a more palliative option in Crohn’s disease, aimed at symptom control rather than cure.
Join an IBD Clinical Trial Near You

Differentiating between Ulcerative Colitis vs Crohn’s disease can be difficult, especially when looking at symptoms alone. To help distinguish between them, healthcare providers must take a deeper look at the location of inflammation, the affected intestinal layers, and the related complications.
Do you have one of these forms of IBD? If so, this can be your chance to help advance scientific research. By joining a clinical trial, you can improve treatment options and quality of life for those with IBD (like yourself!).
There might not currently be a cure for Crohn’s or Ulcerative Colitis disease, but that doesn’t mean there never will be. Ongoing research continuously evaluates better ways to study, treat, and prevent the condition in a wide range of patients.
Learn more about Tandem Clinical Research today. We’ll help you qualify for upcoming trials near you hosted by reputable research facilities, hospitals, and universities.






