
Dealing with medical challenges like Gastroesophageal Reflux Disease (GERD) can feel like navigating turbulent waves. This chronic condition, commonly known as acid reflux, affects millions globally, disrupting comfort and well-being. GERD’s complexity lies in its multifactorial cause rooted in lifestyle habits, genetic predisposition, and physiological factors. In this guide, we will provide insight into GERD’s nature, causes, and management, leading to smoother seas and enhancing quality of life. By understanding GERD, those affected regain control, continuing their voyage with renewed confidence and vitality.
What is GERD?
Gastroesophageal Reflux Disease (GERD) is a medical condition characterized by the backward flow of stomach acid into the esophagus. It manifests as frequent heartburn, chest pain, hoarseness, and coughing. In severe cases, painful swallowing or breathing difficulties may occur. It is important to note that GERD is diagnosed when symptoms occur more than twice a week.
While heartburn is a common symptom of acid reflux, not all heartburn cases are caused by GERD. Heartburn occurs when stomach acid irritates the esophageal lining, resulting in a burning sensation. On the other hand, acid reflux refers to the movement of stomach acid into the esophagus, which can cause tissue damage.
Understanding the triggers of acid reflux is crucial as it is the primary cause of GERD. Common triggers include overeating, consumption of certain foods (such as spicy or fried foods), smoking, alcohol consumption, certain medications, and medical conditions that weaken the lower esophageal sphincter (LES), like hiatal hernia.
If you experience any of these signs or symptoms, it is important to consult a healthcare professional, as they can resemble those of other medical conditions.
Common Symptoms of GERD
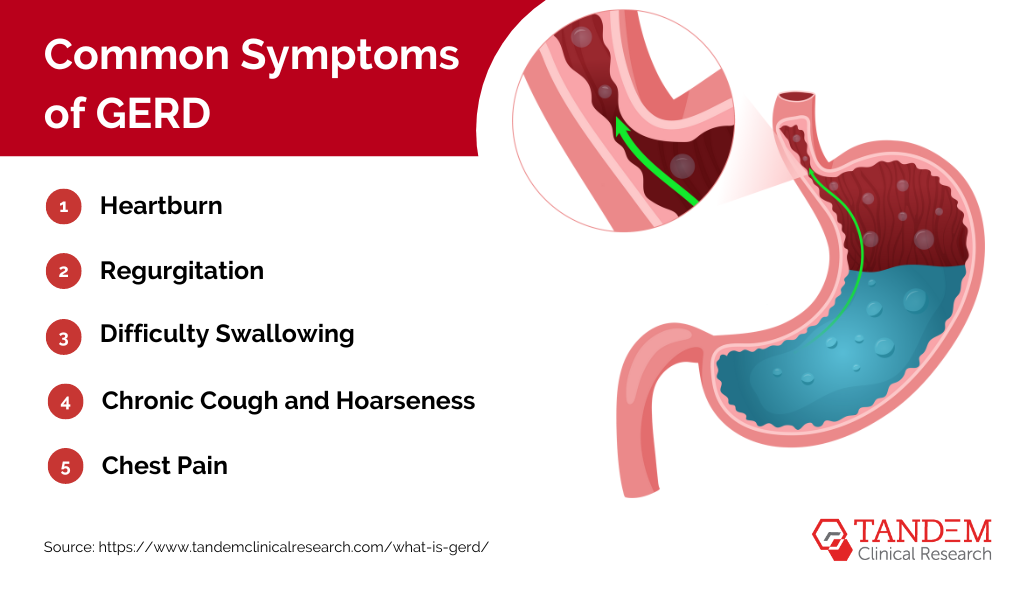
Common symptoms of GERD comprise a range of discomforting and potentially disruptive experiences. Below are the most frequent symptoms:
1. Heartburn: A burning sensation in the chest, usually behind the breastbone, is the hallmark symptom of GERD. It often occurs after eating, especially when lying down or bending over.
2. Regurgitation: The sour or bitter taste of stomach acid that rises in the throat or mouth.
3. Difficulty Swallowing: Known as dysphagia, this can occur when acid damages the esophagus.
4. Chronic Cough and Hoarseness: Stomach acid irritating the throat and airways can lead to persistent cough and voice changes.
5. Chest Pain: Although less common, chest pain can mimic heart-related issues and is often described as a sharp, squeezing discomfort.
Causes and Risk Factors
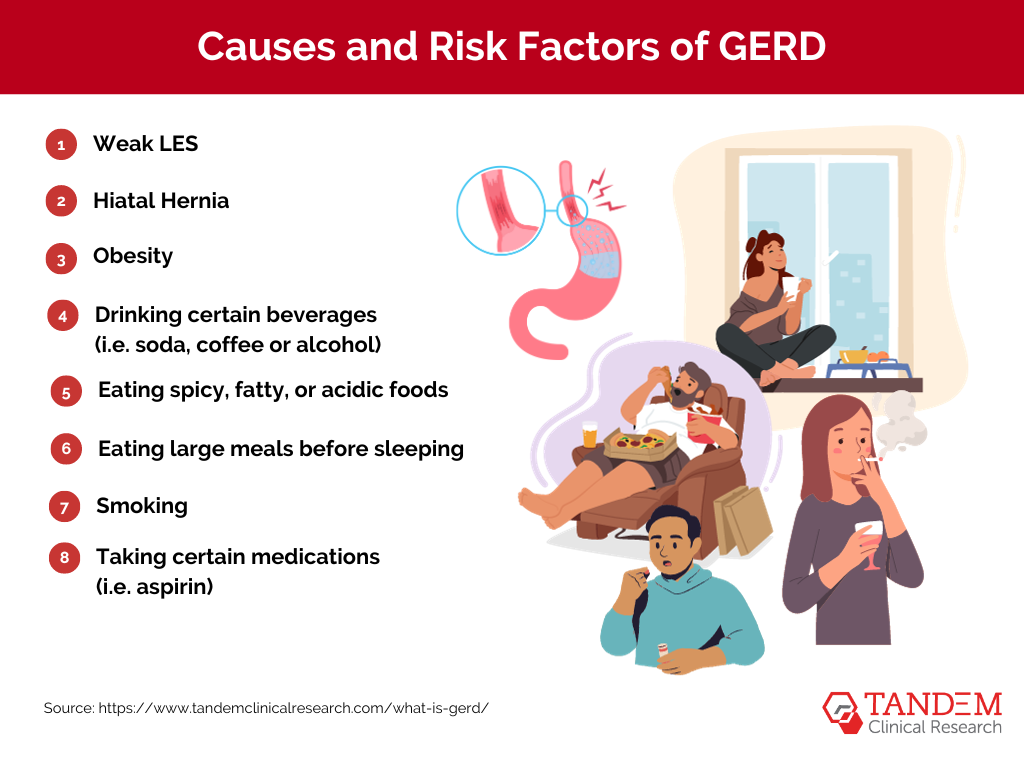
GERD can be influenced by various factors. It is crucial to have an understanding of these factors and proactively take measures to manage and prevent the occurrence of GERD.
Discover the underlying causes and risk factors associated with GERD listed below:
1. Weak LES: A weakened or relaxed LES is widely recognized as the primary cause of GERD. This condition occurs when the LES, a ring of muscle at the bottom of the esophagus, fails to close properly, allowing stomach acid and other digestive fluids to flow back into the esophagus. Understanding the role of the LES in GERD can help guide treatment options and management strategies for individuals experiencing this condition.
2. Hiatal Hernia: This condition, known as hiatal hernia, occurs when the upper part of the stomach pushes through the diaphragm, a large muscle that separates the chest cavity from the abdomen. As a result, the opening in the diaphragm allows acid to flow into the esophagus more easily, leading to symptoms such as heartburn and acid reflux.
3. Obesity: Excess body weight, particularly around the abdomen, increases the pressure on the stomach, which in turn can contribute to the development of acid reflux. This occurs when the lower esophageal sphincter, a muscular valve that normally prevents stomach acid from flowing back into the esophagus, becomes weakened or compromised. The added weight exerts an additional force on the stomach, potentially causing the acid to escape and irritate the sensitive lining of the esophagus. Therefore, maintaining a healthy weight is crucial in reducing the risk of experiencing acid reflux symptoms.
4. Dietary Factors: Consumption of trigger foods such as spicy, fatty, or acidic foods, as well as beverages containing caffeine and alcohol, can exacerbate symptoms of GERD. These foods and drinks have been known to relax the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus, leading to discomfort and heartburn. It is important to be mindful of these triggers and make dietary choices that promote digestive health.
5. Smoking: Smoking can weaken the LES, a muscle that helps prevent stomach acid from refluxing into the esophagus. Additionally, smoking can impair saliva production, which plays a vital role in neutralizing stomach acid and protecting the esophageal lining. By undermining these natural defense mechanisms, smoking increases the risk of acid reflux and related complications.
Complications and Long-Term Effects of GERD

While GERD is a common, treatable condition, understanding its potential risks and complications underscores the importance of seeking professional medical advice if symptoms persist. Early diagnosis and effective management can significantly reduce the progression to these severe outcomes, enhancing the quality of life and ensuring better long-term health. Below are some of the potential complications associated with GERD:
Erosive Esophagitis and Esophageal Strictures
Persistent and untreated GERD can lead to serious complications resulting from the ongoing assault of stomach acid on the delicate tissues of the esophagus. Chronic inflammation, a consequence of this continuous exposure, can cause damage to the esophageal lining, leading to a condition known as erosive esophagitis. This condition often manifests as painful sores or ulcers that can bleed and cause difficulty swallowing.
Strictures, or a narrowing of the esophagus, can also occur as a result of the scarring process after healing from chronic inflammation. This can lead to difficulty in swallowing food and an increased risk of choking. Moreover, chronic GERD increases the risk of developing Barrett’s esophagus, a precancerous condition characterized by abnormal changes in the cells lining the esophagus.
Barrett’s Esophagus and Increased Risk of Esophageal Cancer
Barrett’s esophagus is a condition where the normal, squamous cells lining the esophagus begin to be replaced with columnar cells akin to those found in the stomach or intestines. This cellular change is the body’s way of protecting the esophagus from the damaging effects of acid reflux. However, this adaptation increases the risk of developing esophageal adenocarcinoma, a type of esophageal cancer.
Although the risk of progression from Barrett’s esophagus to esophageal cancer is low, the overall prognosis of esophageal cancer remains poor due to late-stage diagnosis. Therefore, individuals diagnosed with Barrett’s esophagus require regular surveillance via endoscopy to detect any signs of progression towards cancer at an early stage, enabling timely intervention.
Diagnosis of GERD

Diagnosing GERD typically involves a comprehensive approach, which includes gathering a detailed medical history, conducting a thorough symptom assessment, and performing specific diagnostic tests. These tests are designed to provide a more accurate and comprehensive evaluation of the condition. Some of the commonly employed diagnostic tests for GERD include:
1. Endoscopy: A flexible tube with a camera is inserted through the mouth to examine the esophagus for damage.
2. pH Monitoring: This test measures the acidity levels in the esophagus over 24 to 48 hours.
3. Esophageal Manometry: It assesses the function of the esophagus and LES by measuring pressure.
By utilizing these diagnostic tools, healthcare professionals can gain valuable insights into the severity and underlying causes of GERD, enabling them to develop an effective treatment plan tailored to each individual patient’s needs.
Treatment Options
Treatment options for GERD focus on addressing symptoms, promoting healing of esophageal damage, and preventing potential complications. Some of the commonly employed approaches include:
1. Lifestyle Changes: Adopting a healthy diet, maintaining a healthy weight, and avoiding trigger foods can help reduce symptoms.
2. Medications: Over-the-counter antacids, H2 blockers, and proton pump inhibitors (PPIs) can help control acid production.
3. Surgery: In severe cases or when medications fail, surgical procedures like fundoplication may be recommended to strengthen the LES.
It is important to work closely with healthcare professionals to determine the most suitable treatment plan based on individual needs and the severity of symptoms.
Lifestyle Changes for Managing GERD

Lifestyle changes are crucial for managing GERD, as they can reduce symptoms and promote healing, improving overall quality of life. Here are some key modifications to consider:
- Dietary Modifications: Identify and avoid trigger foods to lessen symptoms. Eating smaller, frequent meals can also help reduce acid reflux.
- Weight Management: Maintaining a healthy weight reduces the risk of developing GERD. Excess weight puts additional pressure on the stomach, increasing the chances of acid reflux.
- Quit Smoking: Quitting smoking can significantly reduce symptoms. Smoking weakens the muscles at the lower end of the esophagus and increases stomach acid production.
- Improve Posture: Avoid bending over or lying down after eating. Maintain an upright posture for at least three hours after a meal.
- Elevate Head While Sleeping: Placing a few extra pillows under the head while sleeping helps keep stomach acid in its place and prevents reflux.
Combining lifestyle changes with medications can effectively reduce GERD symptoms, allowing individuals to regain control of their health and lead more comfortable lives. Consult with healthcare professionals when making changes or adjusting medications.
Recent Breakthroughs in Heartburn Research
Clinical research on heartburn and GERD has yielded several noteworthy advancements:
- Understanding Triggers: Research has identified specific dietary triggers, such as caffeine, alcohol, spicy foods, and high-fat meals, which can exacerbate heartburn symptoms. These findings have led to practical dietary recommendations for individuals with heartburn.
- Lifestyle Modifications: Studies have emphasized the importance of lifestyle changes, such as weight management, elevating the head during sleep, and not lying down immediately after meals, in alleviating heartburn symptoms.
- Pharmacological Interventions: Clinical trials have assessed the effectiveness of various medications, including antacids, H2 blockers, and proton pump inhibitors (PPIs), in controlling acid production and providing symptom relief.
- Surgical Innovations: Research has explored surgical options, such as laparoscopic fundoplication, for individuals with severe or refractory GERD. These minimally invasive procedures aim to strengthen the lower esophageal sphincter (LES).
Ongoing Areas of Research
The journey of understanding and managing heartburn is far from over. Current areas of research include:
- Long-term Safety of PPIs: Given the widespread use of PPIs for GERD management, researchers are investigating potential long-term side effects and safety concerns associated with prolonged PPI use.
- Development of Novel Medications: Scientists are working on innovative medications that target different aspects of acid reflux, potentially providing alternative treatment options.
- Precision Medicine: Personalized approaches to managing heartburn are gaining traction, with researchers exploring genetic and molecular factors influencing an individual’s treatment response.
- Esophageal Health: Ongoing research is aimed at understanding the impact of chronic acid reflux on the esophagus and developing strategies to prevent complications such as Barrett’s esophagus, a precursor to esophageal cancer.
Participating in Clinical Trials
If you or someone you know suffers from heartburn or GERD, participating in clinical trials related to these conditions can be a valuable contribution. Clinical trials not only help advance medical knowledge but also offer participants access to cutting-edge treatments and therapies.
Clinical research drives our evolving understanding of heartburn and GERD. With each breakthrough, we move closer to more effective treatments, improved diagnostics, and better management strategies. If you are dealing with chronic heartburn or GERD, it’s essential to stay informed about the latest research findings and consult with healthcare professionals who can provide guidance and tailored treatment plans. The ongoing quest for heartburn relief offers hope for a brighter, more comfortable future for those affected by these conditions.
Would you like to take an active role in your own healthcare by participating in Tandem Clinical Research’s clinical trials? Your involvement could potentially help you gain access to cutting-edge medical treatments while advancing our understanding of heartburn and GERD. Explore the possibilities and join us on this journey toward creating a healthier future.






