Osteoarthritis and osteoporosis are both musculoskeletal conditions that are associated with aging – but although they may seem similar, these conditions are not the same.
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage in joints, which can cause significant pain and stiffness. Osteoporosis, on the other hand, is characterized by low bone density and increased risk of fractures due to bone weakening.
According to the CDC, osteoarthritis affects over 32.5 million adults in the United States, and osteoporosis affects approximately 10 million individuals – the majority of whom are females.
Understanding the difference between the two conditions is crucial when it comes to obtaining an accurate diagnosis and starting the right treatment. Let’s take a deeper look at osteoporosis vs osteoarthritis and their respective challenges.
Understanding Osteoarthritis
Osteoarthritis (OA) is a common and chronic joint disorder characterized by the degeneration of joint cartilage and the underlying bone. It often affects weight-bearing joints such as the knees, hips, spine, and hands, but it can occur in any joint.
Researchers do not fully understand the exact cause of OA, but it is believed to involve a combination of factors, including aging, genetics, joint injury, obesity, and mechanical stress on the joints over time.
In short, as cartilage wears away, joints become stiff, painful, and less flexible.
Over time, bone spurs may also develop around the affected joint, further contributing to pain and reduced mobility.
Risk Factors
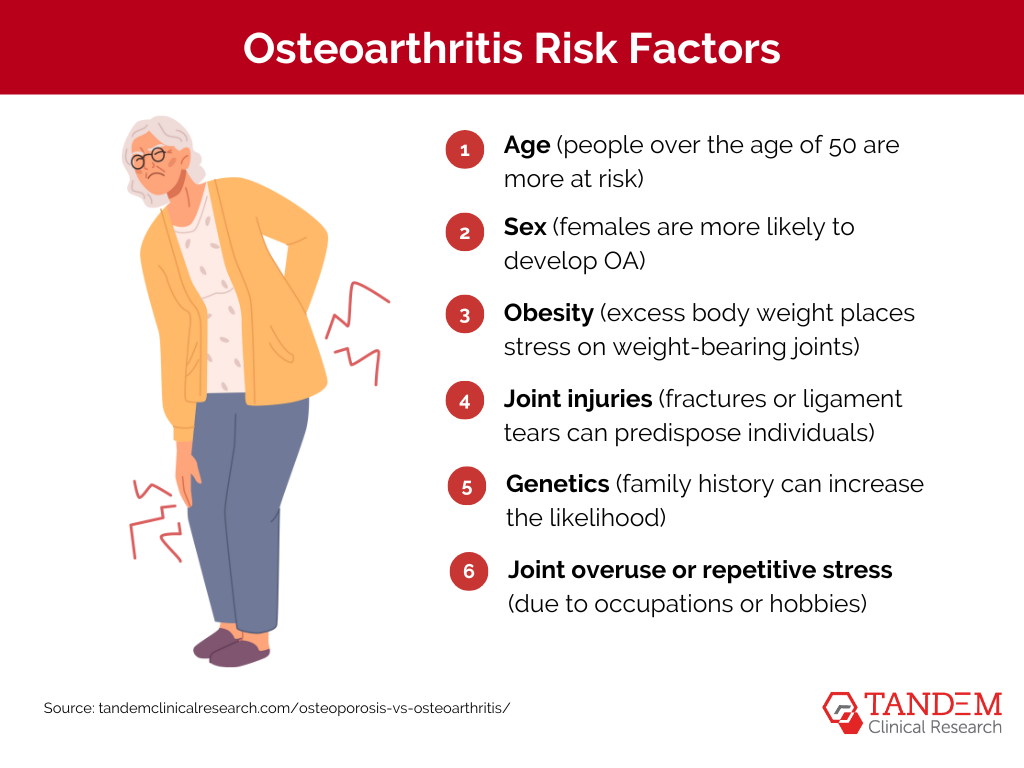
Several factors can increase the risk of developing osteoarthritis, including…
- Age (people over the age of 50 are more at risk)
- Sex (females are more likely to develop OA)
- Obesity (excess body weight places stress on weight-bearing joints)
- Joint injuries (fractures or ligament tears can predispose individuals)
- Genetics (family history can increase the likelihood)
- Joint overuse or repetitive stress (due to occupations or hobbies)
Certain medical conditions, such as rheumatoid arthritis, gout, and metabolic disorders, can also increase the risk of developing OA, as can joint deformities.
Common Symptoms
Although different patients may experience a range of osteoarthritis symptoms, the most common symptoms include:
- Persistent or intermittent joint pain
- Joint stiffness or instability
- Joint swelling
- Functional limitations
- Muscle weakness

In general, osteoarthritis can also contribute to a decreased quality of life. Impaired physical function, chronic pain, and limitations can hold individuals back and result in emotional distress.
Diagnosis & Treatment
Healthcare providers typically diagnose osteoarthritis through a combination of clinical evaluation, medical history assessment, and laboratory tests. Imaging studies such as X-rays, MRI scans, or CT scans can also help them visualize joint damage, cartilage loss, and bone abnormalities.
In some cases, the healthcare provider may perform a joint fluid analysis (arthrocentesis) to rule out other causes of joint symptoms, such as infection or gout.
There is currently no cure for osteoarthritis. Therefore, most treatment options can only aim to alleviate pain, improve joint function, and enhance quality of life.
Healthcare providers will usually recommend a combination of lifestyle modifications, physical therapy, and, in some cases, surgical interventions (such as joint replacement). Medications commonly used to manage OA symptoms include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, corticosteroid injections, and topical analgesics.
How Can You Manage Osteoarthritis?
Although there is no cure for OA, effective management strategies can help alleviate pain, improve joint function, and enhance the quality of life. Here are some actionable steps to manage osteoarthritis:
Lifestyle Modifications
Maintain a Healthy Weight
Reducing excess weight can significantly alleviate the stress on weight-bearing joints, mainly the knees and hips. Even a small amount of weight loss can make a noticeable difference in symptom relief.
Regular Exercise
Incorporate low-impact exercises into your routine – such as swimming, walking, or cycling to maintain joint flexibility and strengthen the muscles around the joints. Regular physical activity can also help with weight management and overall health.
Diet and Nutrition
Anti-Inflammatory Foods
Add anti-inflammatory foods into your diet, such as fatty fish rich in omega-3 fatty acids, fruits, vegetables, nuts, and seeds. These can help reduce inflammation and joint pain.
Supplements
Consider supplements such as glucosamine and chondroitin, which may help support joint health. Be sure to consult with your healthcare provider before starting any new supplement regimen.
Self-Care Practices
Hot and Cold Therapy
Apply heat to relax muscles and improve blood flow or cold packs to reduce swelling and numb the pain. Alternating between hot and cold therapy can also be effective in managing symptoms.
Rest and Recovery
Balance activity with rest to avoid overworking the affected joints. Make sure you get adequate sleep and take breaks during activities to prevent joint strain.
By implementing these management strategies, you can improve their symptoms and maintain a higher quality of life. Regular follow-ups with healthcare providers and adjustments to the treatment plan can help manage osteoarthritis effectively over time.
Understanding Osteoporosis
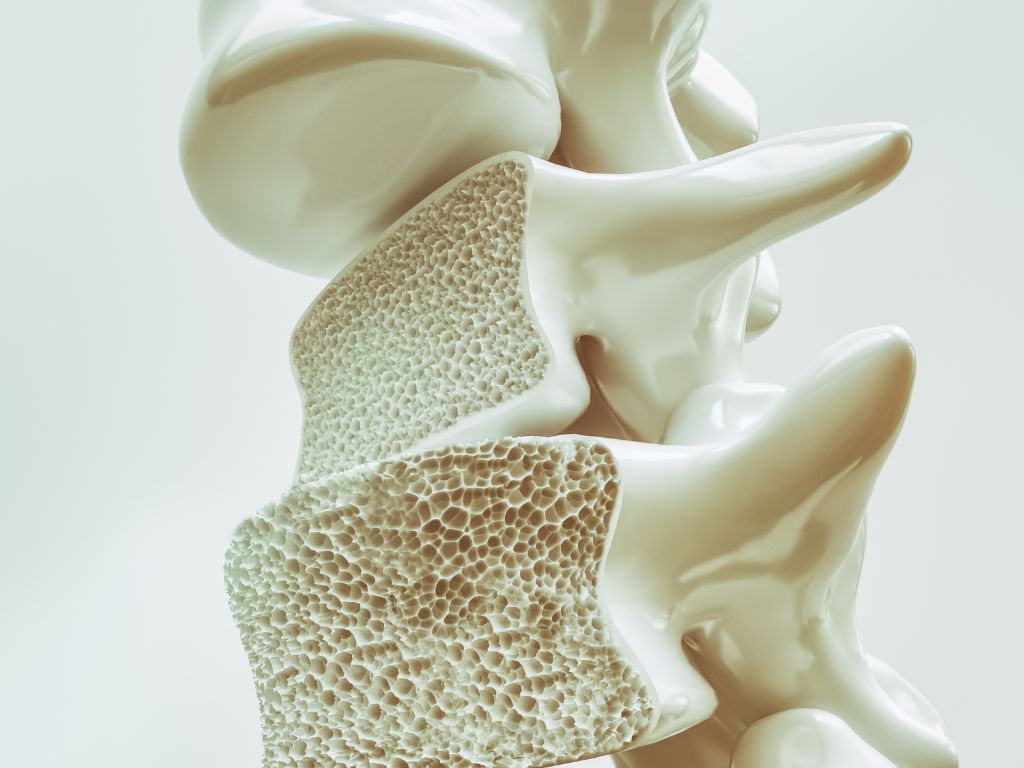
Osteoporosis is a systemic skeletal disorder characterized by low bone mass and microarchitectural deterioration of bone tissue. This increases bone fragility and susceptibility to fractures.
Osteoporosis primarily affects trabecular bone – the spongy, inner part of bones – but it can also involve cortical bone, the outer, denser layer. While the condition can occur in any bone, fractures most commonly occur in the spine, hip, and wrist.
The impacts of osteoporosis can be severe, leading to significant morbidity, disability, and mortality. Fractures resulting from osteoporosis, particularly in the hip and spine, can also have longstanding consequences.
Risk Factors
One in two females will break a bone in their lifetime due to osteoporosis. For females, the incidence is greater than that of heart attack, stroke, and breast cancer combined.
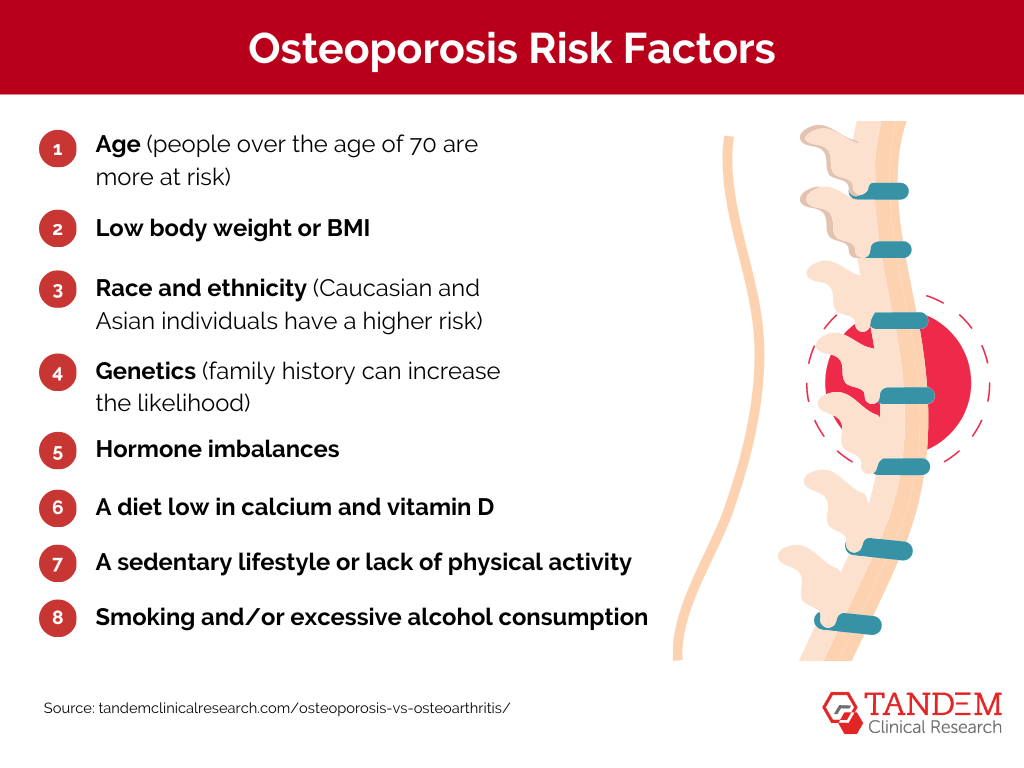
Besides being a female, there are other risk factors for developing osteoporosis, including…
- Age (people over the age of 70 are more at risk)
- Low body weight or BMI
- Race and ethnicity (Caucasian and Asian individuals have a higher risk)
- Genetics (family history can increase the likelihood)
- Hormone imbalances
- A diet low in calcium and vitamin D
- A sedentary lifestyle or lack of physical activity
- Smoking and/or excessive alcohol consumption
Additionally, certain medications can increase your risk of developing osteoporosis – particularly the long-term use of corticosteroids, thyroid medications, and some anticonvulsant medications.
Conditions such as rheumatoid arthritis, hyperthyroidism, celiac disease, and gastrointestinal disorders can also contribute to bone loss and increase the risk of osteoporosis.
Common Symptoms

Osteoporosis is often referred to as a “silent disease,” as it can progress without noticeable symptoms. However, common symptoms of osteoporosis can include:
- Persistent or sudden back pain
- Loss of height due to vertebral compression fractures
- Fractures (especially in the hip, spine, or wrist)
- Rounded shoulders
- Decreased grip strength
- Loss of tooth height
- Bone deformities
Many individuals with osteoporosis may not experience symptoms until they suffer a fracture. Therefore, early detection through bone density testing (DEXA scan) and preventative measures is critical.
Diagnosis & Treatment
Diagnosing osteoporosis typically involves a combination of clinical assessment, bone mineral density (BMD) testing, and evaluation of fracture risk factors.
Bone mineral density testing, commonly performed using dual-energy X-ray absorptiometry (DEXA) scans, measures bone density in key skeletal sites. This test helps determine bone strength and assess the risk of fractures.
Additionally, blood tests may be conducted to evaluate levels of certain markers related to bone turnover and to rule out other medical conditions that can affect bone health.
Although there is no cure, treatment of osteoporosis aims to prevent fractures, preserve bone density, and improve overall bone health. This often involves a multifaceted approach, including lifestyle modifications, such as muscle-strengthening exercises and upping calcium and vitamin D intake through diet and supplements.
Medications are also commonly prescribed to reduce the risk of fractures and improve bone density, such as bisphosphonates, denosumab, selective estrogen receptor modulators (SERMs), hormone therapy (estrogen therapy), and parathyroid hormone analogs.
Most healthcare providers make treatment decisions for osteoporosis based on a range of factors, including the patient’s age, fracture risk, bone density levels, and overall health. Regular monitoring and follow-up evaluations are also essential to assess treatment effectiveness and make necessary adjustments.
How Can You Manage Osteoporosis?
Management of osteoporosis involves a combination of lifestyle changes, dietary modifications, medications, and regular medical check-ups. Here are some actionable steps to help manage osteoporosis:
Diet and Nutrition
Calcium-Rich Foods
Stick to a diet that includes plenty of calcium-rich foods such as dairy products, leafy green vegetables, almonds, and fortified foods. Adequate calcium intake is essential for bone health.
Vitamin D
Vitamin D helps your body absorb calcium. Get enough vitamin D through sunlight exposure, fortified foods, or supplements if necessary. Fatty fish, egg yolks, and fortified milk are good sources.
Exercise and Physical Activity
Weight-Bearing Exercises
Consider implementing weight-bearing exercises such as walking, jogging, or dancing. These activities help build and maintain bone density.
Strength Training
Incorporate strength training exercises into your routine to improve muscle mass and bone strength. Lifting weights or using resistance bands can be effective.
Lifestyle Modifications
Avoid Smoking and Limit Alcohol
Smoking and excessive alcohol consumption can weaken bones. Avoid smoking and limit your alcohol intake to reduce the risk of osteoporosis-related fractures.
Fall Prevention
Take proper measures to prevent falls in your home – like installing railings. Make sure your living space is well-lit, remove tripping hazards, and use assistive devices if needed.
Regular Medical Check-Ups
Bone Density Tests
Schedule regular bone density tests (DEXA scans) to monitor your bone health and assess the effectiveness of your treatment plan.
Consultation with Healthcare Providers
Make regular appointments with your healthcare provider to discuss your osteoporosis management plan, any new symptoms, and adjustments to your treatment as necessary.
Managing osteoporosis requires a proactive and comprehensive approach. By combining a healthy diet, regular exercise, lifestyle changes, medication adherence, and consistent medical monitoring, you can maintain bone health and reduce the risk of fractures, leading to a better quality of life.
Key Differences Between Osteoarthritis & Osteoporosis

Affected Areas
Osteoarthritis primarily affects the joints, particularly those that bear weight such as knees, hips, spine, and hands. Osteoporosis affects the bones, decreasing bone density over time, especially in the spine, hip, and wrist bones.
Symptoms
Although some symptoms may overlap between these conditions, osteoarthritis primarily affects the joints, causing swelling, stiffness, pain, or even crepitus (a grating or crackling sensation).
In contrast, the symptoms of osteoporosis are related to decreased bone density, likely presenting in back pain, loss of height, decreased strength, etc.
Diagnostic Methods
There are similarities in the diagnostic process for osteoarthritis and osteoporosis, but they are not usually diagnosed in the same way.
OA diagnosis typically involves clinical evaluation, imaging studies, and sometimes joint fluid analysis. In contrast, osteoporosis diagnosis includes clinical assessment, bone mineral density testing, evaluation of fracture risk factors, and blood tests to assess bone health and rule out other conditions.
Overlapping Factors & Comorbidities
Certain conditions can coexist with both osteoarthritis and osteoporosis. This can complicate the diagnostic process and make it difficult for healthcare providers to treat the root problems.
For instance, rheumatoid arthritis (RA) is an autoimmune disorder that can affect joints, causing inflammation, pain, and joint damage similar to OA. However, RA primarily targets the synovium, causing erosive changes in the joint structure, whereas OA involves degenerative changes in cartilage and bone.
Additionally, it can be difficult to distinguish between fractures resulting from osteoporosis-related bone fragility and those associated with OA-related joint degeneration.
These overlapping conditions highlight the complexity of diagnosing and managing musculoskeletal disorders, particularly because multiple conditions can coexist. Healthcare providers must carefully assess symptoms, perform thorough evaluations, and use the appropriate diagnostic tests to accurately identify underlying conditions and tailor treatment plans.
The Importance of Early Diagnosis & Intervention

The earlier your healthcare provider catches osteoarthritis or osteoporosis, the better quality of life you will likely experience as you age.
Early detection allows for the timely implementation of essential management strategies, including lifestyle modifications, medications, and rehabilitative therapies, all of which can help alleviate symptoms and prevent further complications.
Furthermore, early intervention can slow the progression of these conditions, reducing the risk of irreversible joint damage, disability, and fractures.
If you’ve experienced any of the symptoms associated with OA or osteoporosis, or if you think you may be at risk, don’t wait: contact your healthcare provider immediately.
Clinical Trials for Osteoarthritis or Osteoporosis
When it comes to learning about these two conditions and developing treatment plans, clinical trials provide much-needed insight to researchers. Their goal is to evaluate the safety and efficacy of new interventions and medications, changing how we diagnose and treat musculoskeletal conditions.
By enrolling in a safe, professional clinical trial for osteoarthritis or osteoporosis, you can help scientists gather valuable data on treatment outcomes, side effects, and long-term effects. This information contributes to medical advancements that can benefit you and others who wind up in similar situations.
Get Matched With Tandem Clinical Research Today
Osteoarthritis and osteoporosis are distinct musculoskeletal conditions with unique characteristics and impacts. While these conditions have different pathologies, they can often coexist and share risk factors – which makes treating and studying them challenging.
Tandem Clinical Research plays a crucial role in matching patients with clinical trials for OA and osteoporosis, helping individuals gain access to innovative treatments and contributing to advancements in musculoskeletal research.
By participating in clinical trials with Tandem Clinical Research, you have the opportunity to receive cutting-edge therapies under close medical supervision while also contributing to the development of new treatment options.
To find out if you qualify for a study in Louisiana, New York City, or central Florida, get in touch with Tandem Clinical Research today.
Updated: September 2, 2024
